|
| By: Silmara Mansur |
By Cristiane Albuquerque
With 66,000 new cases of breast cancer in 2020, according to projections by the National Cancer Institute (INCA), policies for diagnosing the disease in Brazil are mired in an unresolved controversy. A lack of clarity related to the minimum age for undergoing mammograms puts the Unified Health System (SUS) and the private sector on opposite sides, exposing historical differences in their respective views on the diagnostic technique. In an extremely unequal country, disagreements over the use of this exam as a screening technique resulted in a parallel system for early detection, in which Brazilian women who pay for a health plan have easier access to the procedure than those who use the public healthcare service.
The clashes regarding this issue resulted, in practice, in two distinct programs for breast cancer prevention, highlighting the tension between the public and private sectors: one system designed for the middle class, which uses health plans, and another designed for the poorest classes, typical SUS users.
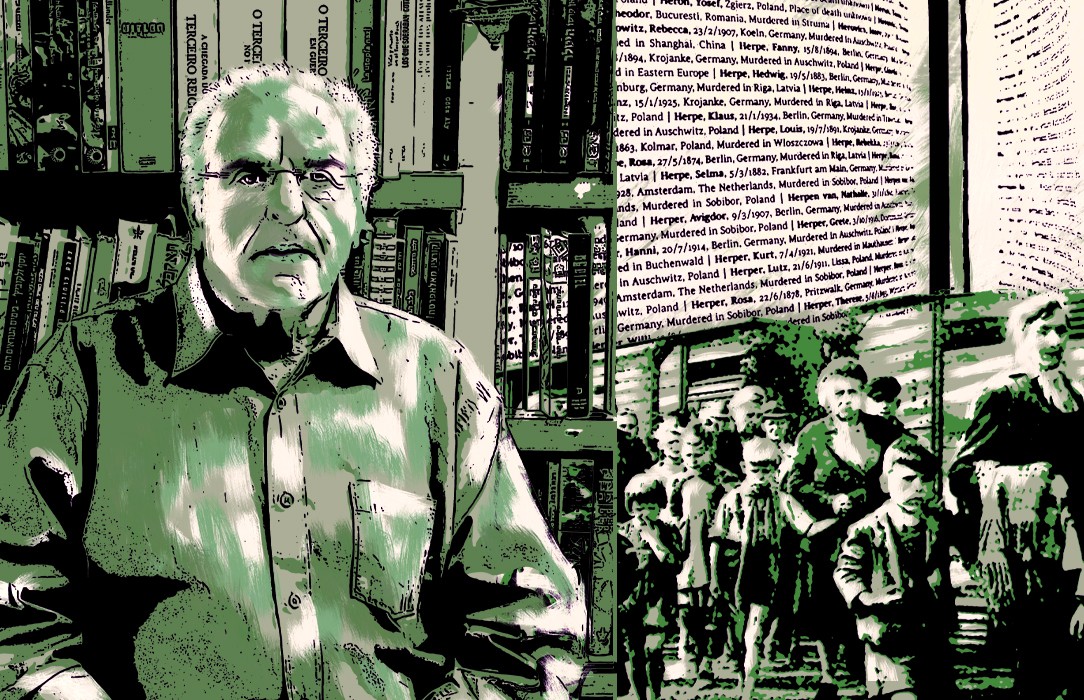
The process of incorporating mammography as a diagnostic tool and the debates on the implementation of screening programs in Brazil were studied by researchers Luiz Antonio Teixeira and Luiz Alves, from the Casa de Oswaldo Cruz, authors of the article Still Controversial: Early Detection and Screening for Breast Cancer in Brasil, 1950-2010, published in the scientific journal Medical History. “The differing perspectives on the subject reflect tensions between the desire to implement the constitutional right to healthcare for all and the reality of dramatic social inequality and stratified access to healthcare. These difficulties are also related to the strength of the private sector in defining public health actions and the inability of the public sector to regulate them,” emphasizes Luiz Antonio Teixeira.
According to the researchers, the clashes regarding this issue resulted, in practice, in two distinct programs for breast cancer prevention, highlighting the tension between the public and private sectors: one system designed for the middle class, which uses health plans, and another designed for the poorest classes, typical SUS users.
In the context of the structuring of the Unified Health System (SUS), in 1990 the National Cancer Institute (INCA) established its position as the institution responsible for organizing cancer screening policies. However, there were limitations on the ability to implement the recommendations of the Institute, especially in relation to the strongly structured private sector, which defended wide use of mammograms.
"The alignment of INCA with PAHO (the Pan American Health Organization), the face of the World Health Organization (WHO) in the Americas, resulted in policies that took into account the epidemiological complexity and socioeconomic inequality of each region, for example," said Luiz Alves, a historian and postdoctoral fellow in the Postgraduate Program in the History of Sciences and Health at the COC, who also authored the article.
In a law approved in 2008 by the Brazilian Congress, mammography exams were guaranteed to all women aged 40 and over. Openly contrary to this law, in 2015 INCA established new guidelines for detection of early breast cancer with a recommendation of mammograms for women between 50 and 69, every two years.
It is important to point out that each group positioned itself based on its own expectations, interests and values. The problem, in a practical sense, is the creation of parallel regimes for early detection, which often contradict each other
In the private sector, the use of mammography is based on the interaction between doctor and patient, a client of the health plan demands that her doctor indicate the most accurate exams possible to assess her health. In public health clinics, poor women have mammograms in accordance with national recommendations. “Those who can afford private insurance make more use of mammography, since the exam is socially recognized as more effective. On the other hand, in the SUS, the relationship between doctor and patient is based on the notion of a user and the right to health, which means that individual demands are governed by the system,” stresses Luiz Alves.
The research, carried out as part of the History of Cancer project, a partnership between Fiocruz and INCA, analyzed medical sources, mainly journals specialized in oncology published between 1950 and 2017, reports from Brazilian Mastology Conferences and Brazilian campaigns for cancer screening, books, institutional documents and oral testimonies from health professionals, patients and associations.
Conflicts of interest
The research also revealed the conflicts of interest between the three predominant views regarding mammograms for screening in Brazil — those defended by medical societies, public health specialists and patient associations — from the 1960s to the 2000s.
Supported by WHO and PAHO guidelines, public health actors pointed to the inadequacy and unfeasibility of carrying out organized national screening programs due to economic inequalities and limited access to health services. On the other hand, members of medical societies, supported by private health specialists, defended the implementation of a policy that would favor mammograms. Patient associations, on the other hand, demanded wide distribution of mammography equipment, a reduction in the age range for starting tests and a greater frequency of exams.
“It is important to point out that each group positioned itself based on its own expectations, interests and values. The problem, in a practical sense, is the creation of parallel regimes for early detection, which often contradict each other, the absence of a resolution and, above all, the limitations imposed on healthcare for the population,” said Luiz Alves.
According to Luiz Antonio Teixeira, the parameters for transforming mammography into an adequate tool for early diagnosis of breast cancer are still uncertain. “This does not depend solely on scientific evidence, but rather on the relative positions of groups with historically constructed, consolidated interests and powers,” he said.
While the perspective of specialist physicians and patient associations is strongly linked to society, for example through advertising campaigns, especially "Pink October," those in public health attribute the position of opponents to the interests of large biomedical corporations. "The discussion remains open, the screening problem translates into an issue within the relationship between technology/science and society: how to manage the tensions between actors with different interests in the face of weak scientific evidence. There is still no proof that screening mammograms have reduced mortality from breast cancer in Brazil,” said Teixeira.
The military dictatorship and the weakening of public health
The economic perspective on health care, a preference for the use of private health services and a weakening the Ministry of Health were some of the consequences pointed out by the study on the impacts on public health, medicine and cancer treatment during the more than 20 years of military dictatorship in Brazil (1964–1985).
Military policy, according to Luiz Alves, prioritized the outsourcing of state health services to the private sector, while the National Cancer Treatment Program (PNCC), created by the Ministry of Health in 1973, operated via reimbursement by the State for all procedures performed in private hospitals and laboratories. “Mainly due to emphasis on the pension system and the development of hospital medicine, the military dictatorship contributed to the weakening of the Ministry of Health at the time. This structuring of the health system greatly favored the private sector, which grew by providing services to the Ministry of Social Security and Assistance,” he explained.
The PNCC also established links between private institutions and the National Cancer Division, an agency of the Ministry of Health, that allowed them to receive equipment for diagnosis and treatment of cancer: mammography equipment and other instruments purchased with public money were delivered to state public networks and, often, to private hospitals and clinics.
From this perspective, the private sector became an organizer in the development of cancer screening policies, hindering the possibility of broad, coordinated actions. “In the case of cancer hospitals, there was already a consolidated model of private institutions, founded by philanthropic organizations, which were supported with public funding. Practically all cancer institutes and hospitals follow this model, with the exception of the National Cancer Institute itself, a State institution,” concluded Alves.
Translated by Naomi Sutcliffe de Moraes